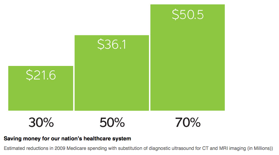
A healthy POCUS program not only conserves resources and is a less expensive way of answering many clinical questions, the POCUS program can also generate revenue. Regardless of the practice setting POCUS studies are billed utilizing CPT codes, just like any other procedure. In fact Adhikari et al. a studied an emergency room with 70,000 visits and found that an active billing practice can generate $350,000 a year.
Medical Liability is an is always a concern in our medical environment. However, when trying to assess data which demonstrated harm to patients from groups of professions performing POCUS, there exists a paucity of data. In fact, as of this writing, a Pubmed search does not return any case studies to demonstrate harm to patients with the implementation of POCUS. In fact, since there is no data on this subject, there are at least 3 studies (POCUS lawsuits Blaivas, POCUS Lawsuits 5, Analysis of lawsuits related to point-of-care ultrasonography in neonatology and pediatric subspecialties) which looked at the number of law suits filed in state and federal court related to POCUS. Over the 20 year period, these authors found law suits related to POCUS in the 20 years studied. in each of these cases, the breach of duty was alleged to be “a failure to perform the bedside sonogram,” thereby violating the standard of care.